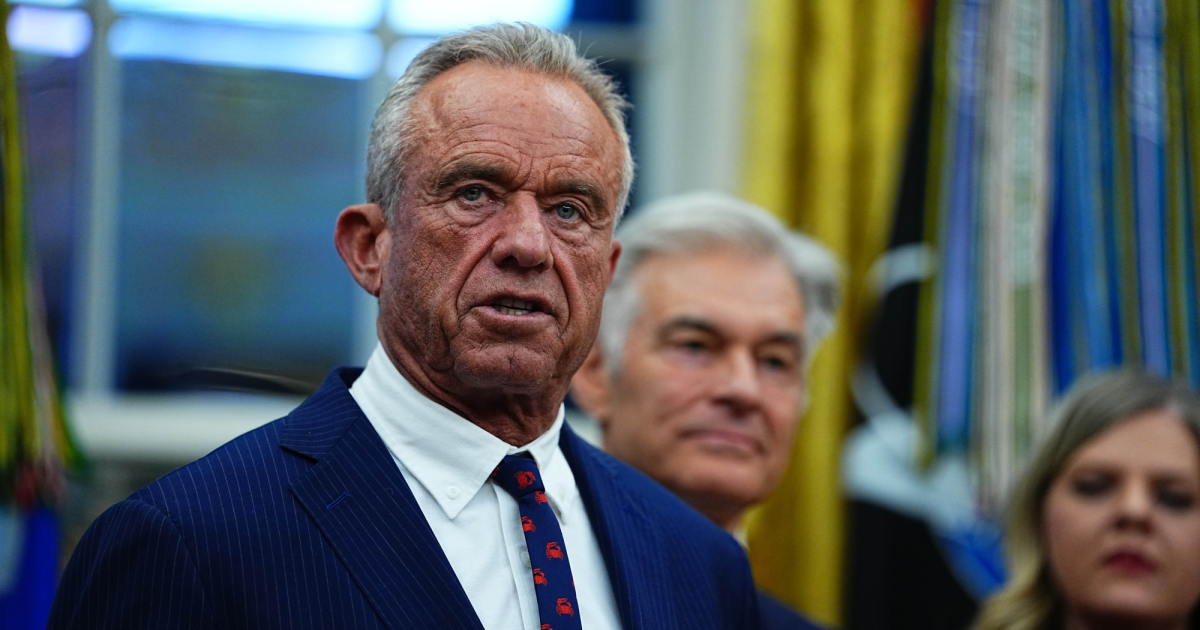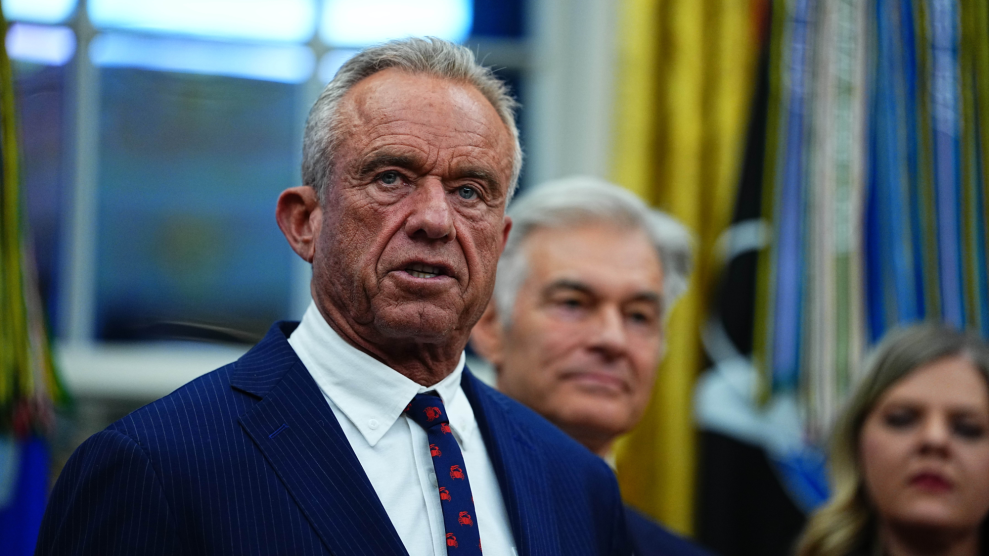
United States Secretary of Health and Human Services Robert F. Kennedy JrAaron Schwartz/Pool/CNP/ZUMA
This article first appeared in WIRED and is published here as part of the Climate Desk collaboration.
The U.S. Department of Health and Human Services (HHS) is in the process of creating a generative artificial intelligence tool designed to analyze data from a national vaccine monitoring database and to produce hypotheses regarding vaccine-related adverse effects, as indicated in an inventory released last week outlining the agency’s AI plans for 2025.
While the tool has not yet been implemented, documentation from HHS reveals it has been in development since late 2023. Experts express concerns that any predictions this tool generates could potentially support HHS Secretary Robert F. Kennedy Jr. in advancing his anti-vaccine stance.
A prominent vaccine skeptic, Kennedy has significantly altered childhood vaccination recommendations during his tenure, removing several vaccines from the list of immunizations recommended for children, including those for Covid-19, influenza, hepatitis A and B, meningococcal disease, rotavirus, and respiratory syncytial virus (RSV).
He has also advocated for a revamp of the existing vaccine injury monitoring system, known as the Vaccine Adverse Event Reporting System (VAERS), arguing that it fails to adequately reflect the true incidence of vaccine side effects. Furthermore, he has suggested modifications to the federal Vaccine Injury Compensation Program that might facilitate lawsuits for adverse events lacking proven ties to vaccines.
VAERS, which is jointly overseen by the Centers for Disease Control and Prevention (CDC) and the Food and Drug Administration, was established in 1990 to identify potential safety issues with vaccines following their approval. Reports of adverse reactions can be submitted to this database by anyone, including healthcare providers and the public. Because the claims are not verified, VAERS data alone cannot be used to ascertain if a vaccine caused an adverse event.
“I would expect, depending on the approaches used, a lot of false alerts and a need for a lot of skilled human follow-through.”
According to Paul Offit, a pediatrician and director of the Vaccine Education Center at Children’s Hospital of Philadelphia, “VAERS, at best, was always a hypothesis-generating mechanism. It’s a noisy system. Anyone can report, and there’s no control group.”
Offit emphasizes that the system merely reflects adverse events that occur following immunization, without establishing a causal link. The CDC’s own site clarifies that a VAERS report does not equate to a vaccine causing an adverse event. Despite this, anti-vaccine activists have historically misinterpreted VAERS data to argue against vaccine safety.
Leslie Lenert, the former founding director of the CDC’s National Center for Public Health Informatics, indicates that government researchers have been employing traditional natural language processing AI models to analyze VAERS data for years; thus, it isn’t unexpected that HHS is moving toward more sophisticated large language models.
A significant drawback of VAERS is its lack of data on the number of individuals vaccinated. This absence can skew the perceived frequency of logged events. Lenert states that correlating VAERS information with other data sources is essential for accurately assessing risks.
Large language models (LLMs) are well-known for generating plausible yet inaccurate information, which emphasizes the necessity for human intervention when evaluating any hypotheses they produce. “VAERS is intended to be exploratory,” says Lenert, now the director of the Center for Biomedical Informatics and Health Artificial Intelligence at Rutgers University. “Some people at the FDA are currently interpreting it as more than exploratory.”
Vinay Prasad, director of the FDA’s Center for Biologics Evaluation and Research, reportedly recommended stricter vaccine regulations in a recent memo, attributing the deaths of at least ten children to the Covid-19 vaccine without providing evidence. These deaths were reported to VAERS and had already been evaluated by FDA personnel. More than a dozen former FDA commissioners expressed their concerns about Prasad’s proposed regulations in a letter published in The New England Journal of Medicine, claiming that such changes could drastically reshape vaccine regulations based on selective evidence interpretation.
Jesse Goodman, an infectious disease physician and professor at Georgetown University, believes that while LLMs may expose previously unidentified vaccine safety issues, the inaccuracies and incompleteness of VAERS data necessitate thorough investigations of any leads generated.
“I would anticipate a number of false alerts and emphasize the need for skilled human follow-up by professionals knowledgeable about vaccines, potential adverse events, and the complexities of LLM outputs,” he notes.
Amid significant staffing reductions at the CDC, Goodman stresses the urgency of having strategies and resources ready to address emerging data, including proper screening and determining which aspects require further research.
Historically, VAERS has identified valid safety concerns, such as cases of a rare clotting disorder linked to the Johnson & Johnson Covid-19 vaccine and instances of myocarditis predominantly among younger males who received the mRNA Covid-19 vaccines.
HHS did not respond to a request for comment.