Artificial intelligence has emerged as a formidable ally in the struggle between medical research and the intricate mechanisms of diseases. Its application is becoming more prominent across research, clinical practices, and healthcare systems. This transition, initially seen as a minor development in recent years, is evolving into a foundational element of future medicine.
AI has consistently demonstrated its potential to analyze and unravel complex biological systems, yielding significant insights that can be transformed into life-saving interventions and personalized treatment strategies—developments that once seemed unimaginable.
A recent study published in December in Nature Communications showcases this potential concerning a well-known group of viruses: herpesviruses (Herpesviridae). While commonly recognized for causing conditions like cold sores, chickenpox, and shingles, some of these viruses are also implicated in cancer.


Identifying Genetic Control Zones
An estimated 90 to 95 percent of adults will be infected with at least one herpesvirus during their lifetime. These viruses are adept at masquerading as “secret agents” within biological systems. They infiltrate epithelial and immune system cells, replicate, and instigate initial infections.
Following this, they enter a dormant phase, hiding in nerve cells or immune lymphocytes until the opportune moment arises. This reactivation can occur during periods of stress, illness, or immune suppression—situations where the immune system is compromised—resulting in various symptomatic diseases.
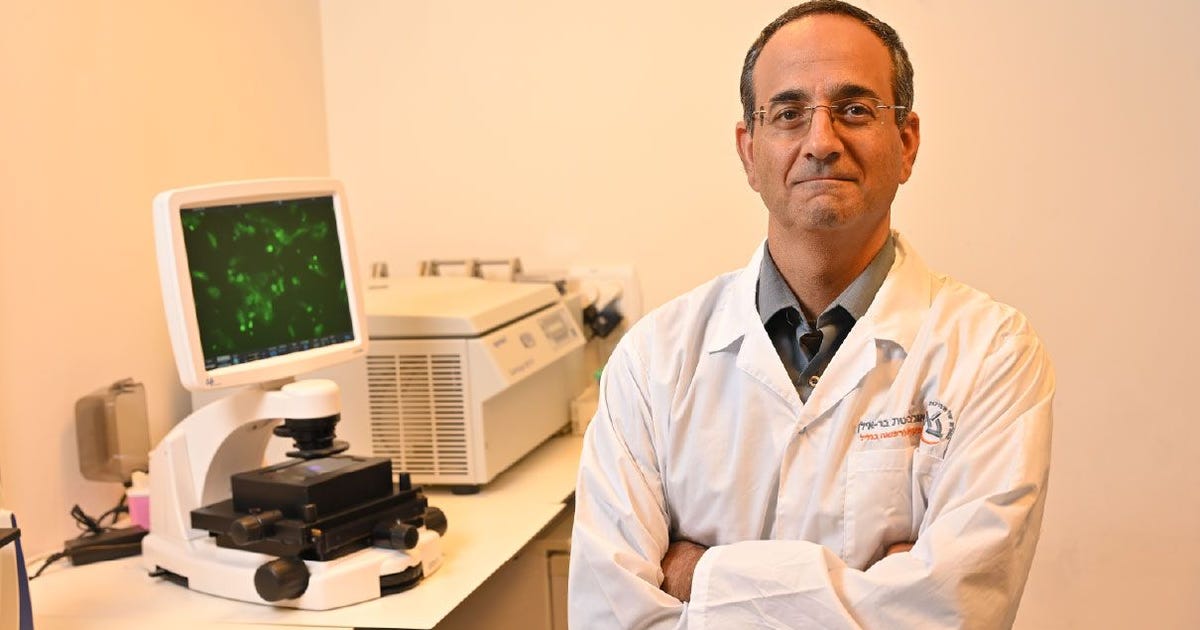
The exact process that prompts herpesviruses to shift from a dormant to an active state has largely remained elusive. However, this new research may shed light on this mystery. Led by Professor Meir Shamay of Bar-Ilan University’s Azrieli Faculty of Medicine, the study has introduced a pioneering AI tool known as ENHAvir.
This model functions akin to how search engines comprehend language; however, instead of words, it identifies genetic control regions—specific DNA segments that trigger gene activation in herpesviruses.
These short DNA segments, referred to as “enhancers,” are crucial in transitioning herpesviruses from a dormant to an active status. As such, researchers believe that pinpointing these control genes might allow for interventions that either suppress or facilitate their activity, potentially preventing disease outbreaks.
At his lab, Professor Shamay studies herpesviruses, focusing on two cancer-causing strains. The first is Kaposi’s sarcoma-associated herpesvirus (KSHV), which is linked to soft-tissue cancers arising from blood or lymphatic vessel cells, and primary effusion lymphoma (PEL). The second is Epstein-Barr virus (EBV), which is present in over 95 percent of adults and can contribute to cancers like lymphoma and gastrointestinal cancer. Professor Shamay elaborates, “We investigate how these viruses induce cancer and aim to uncover the molecular mechanisms at play to develop future treatments and early detection tools.”
Beyond Herpes
Earlier studies in Shamay’s lab had already identified these enhancers as significant contributors to alterations in viral behavior. However, finding them across different positions relative to the regulating gene is complex, especially within the compact viral genomes. “Our previous research allowed us to pinpoint six enhancers in the Kaposi’s sarcoma virus, which led us to hypothesize that we could use sequences from one virus to identify enhancers in others,” explains Shamay.
The challenges of locating these control mechanisms using traditional methods highlight the significant advantages of employing AI in this research. Moreover, it underscores the rapid advancement of AI as a research tool.
“Rather than relying on complex and tedious methods, we employed an AI tool to tackle this puzzle,” says Shamay. “Typically, AI tools are trained on millions of genetic sequences, but we only used six for this model,” he explains.
“Initially, the AI recognized the known enhancers we had already identified, which validated the model’s efficacy. Subsequently, based on the insights it garnered, it identified additional enhancers that were previously unknown. We validated these predictions through laboratory experiments, confirming their accuracy,” adds Shamay.
Utilizing just six sequences, the AI model successfully identified novel enhancers in various herpesviruses, including Epstein-Barr virus and Cytomegalovirus (CMV), which can cause fetal harm, alongside HSV-1 (oral herpes) and HSV-2 (genital herpes). These AI-led discoveries will guide future research into treatments and preventive measures targeting herpesvirus-related diseases—a significant array of conditions.
“This study highlights the capabilities of AI, which enabled us to uncover control regions by learning from just six sequences. Its findings greatly enrich our understanding of herpesvirus mechanisms and extend relevance beyond the viral domain.
“The mechanisms regulating enhancers are also present in the human genome, implying that studying viral enhancers may provide insights into human enhancers. This connection to evolution suggests that viruses have survived for millions of years by extracting essential sequences from human cells. Investigating viral genes through AI opens avenues to understanding the biological systems within the human body,” concludes Shamay.