Recently, Robert F. Kennedy Jr. endorsed the questionable assertion that ketogenic diets can “cure schizophrenia.” While experts contest this idea, budding research indicates that such diets may enhance psychiatric symptoms.
Initial small-scale studies hint that a ketogenic diet—a high-fat, low-carbohydrate regimen that induces ketosis—might benefit individuals grappling with mental health conditions such as depression, schizophrenia, and bipolar disorder.
A Stanford study involving 21 participants undergoing treatment for either bipolar disorder or schizophrenia found that most experienced “clinically meaningful improvement” in their psychiatric symptoms after following a keto diet. Another study, published in JAMA, reported “modest improvements” in subjects with depression who adhered to a keto diet.
A 2019 case study, which Kennedy seemed to reference, observed that two individuals diagnosed with schizophrenia managed to discontinue their antipsychotic medications while on a ketogenic diet. However, Dr. Christopher Palmer, a contributor to the study, stated that Kennedy’s claims about a cure were “not accurate,” emphasizing the need for further investigation.
“While I appreciate Secretary Kennedy’s passion for my research, I have never claimed to cure schizophrenia or any mental disorder, and I do not use the word ‘cure’ in my work,” Palmer expressed to the New York Times.

(Getty Images)
Palmer’s findings indicated that while the two patients who maintained the diet could manage their symptoms, they stood out as exceptions among others who did not achieve similar benefits.
“It’s unfortunate that he used the term cure,” Palmer informed the Harvard Crimson. “If he had merely suggested a powerful treatment, it would have been more accurate.”
The Independent has reached out to the Department of Health and Human Services for their input.
For years, experts have speculated a possible connection between psychiatric symptoms and metabolic conditions, particularly based on research surrounding medication-resistant epilepsy in children.
However, robust scientific studies, particularly involving adult psychiatric patients, are lacking to confirm this suspicion. Preliminary studies tend to be limited in scope and frequently do not incorporate control groups following non-keto diets.
“There’s a seed of truth in this,” remarked Ken Duckworth, the medical director of the National Alliance on Mental Illness, as he shared with the Washington Post. “But the science is still developing.”

(Heather Diehl/Getty Images)
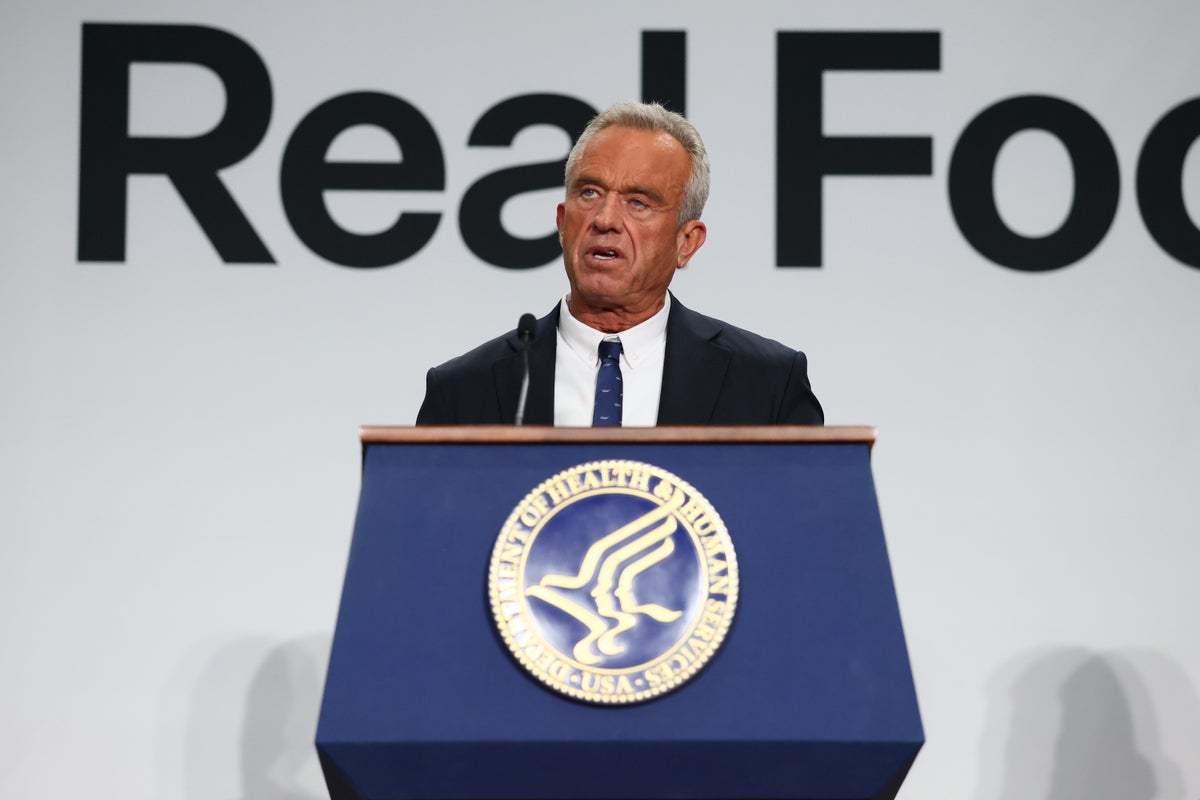
Earlier this month, Kennedy claimed that Palmer’s research indicated keto diets could “cure schizophrenia” while advocating for his “Eat Real Food” initiative. He encourages Americans to cut down on processed foods.
Kennedy’s revised food pyramid recommends increased consumption of meat and saturated fats through whole milk and cheese.
Palmer expressed concern that Kennedy’s unfounded assertion could drive individuals with schizophrenia to abandon their medications and adopt a ketogenic diet.
“That would be disastrous,” Palmer told the Harvard Crimson.