In her recent piece for the New England Journal of Medicine (NEJM), Lisa Rosenbaum, MD, explores the challenges facing U.S. primary care in her article titled Is a Long-Simmering Crisis Boiling Over? U.S. Primary Care Today. While the prevailing sentiment might be an emphatic “Yes,” this perspective is not the only one. Dr. Rosenbaum opens with an illuminating narrative about a physician known as Dr. H:
After completing her internal medicine residency, Dr. H joined a practice in the Midwest, taking over a primary care patient panel from a retiring endocrinologist. Initially, she found the work rewarding, diagnosing and treating a variety of medical conditions, fostering long-term relationships with patients and families, and caring for them in the hospital — until hospitalists emerged. For her, the role of a dedicated internist aligned perfectly with her aspirations. “Lifelong learning and the ability to assist others;” she reminisced, “It was the best job in the world.”
For the past eighteen years, my focus has been on medical education, particularly in cultivating more primary care physicians to serve in rural and underserved regions. But who exactly are these practitioners? Primary care encompasses more than what was once termed the “general practitioner” or GP. [1] Today, core specialties considered primary care include Family Medicine, Internal Medicine, General Surgery, Pediatrics, Obstetrics & Gynecology, and Psychiatry, with Emergency Medicine sometimes falling into this category as well. [2] Remarkably, Emergency Medicine became formally recognized as a specialty only in the 1970s. During my youth, when I needed medical care, the hospital would summon one of my family doctors, who lived nearby and could swiftly attend to my needs.
This historical context might seem recent, but in the rapidly evolving landscape of healthcare, it feels like a different era. Returning to Dr. H:
She only began to realize that the traditional generalist role was in jeopardy some fifteen years later, after moving to a multispecialty practice under a nonprofit foundation. Initially satisfied with her work, Dr. H soon faced mounting pressures in primary care — shorter appointment times, overwhelming inboxes, and staff shortages due to the Covid pandemic — gradually diminishing her effectiveness as a patient’s doctor.
Like many primary care physicians (PCPs), she attempted to cope by increasing her workload. Without adequate staff support, she managed patient intake, took vital signs, and handled scheduling for tests and follow-ups. When leadership threatened to reduce vacation days for late documentation, she began dedicating hours late at night to charting, all while managing responsibilities at home with a young child and a chronically ill spouse. Yet, one obstacle proved insurmountable: the inability to see her patients in their times of need. Prohibited from double-booking appointments to fit them in, she often only learned of patients’ requirements after centralized triage had redirected them to urgent care.
Urgent care facilities are undeniably costly yet have become a necessity in many communities. My experiences with urgent care have proven expensive, raising questions about accessibility. For one of Dr. H’s patients:
A woman suffering from recurrent herpes infections called to request a refill of valacyclovir. Following an algorithm, the staff informed her that a clinic visit was necessary as she hadn’t seen Dr. H in over a year. With no appointments available, she was directed to urgent care, where the clinician refused to prescribe valacyclovir without a culture. Eventually, Dr. H learned of the situation and refilled the medication. However, similar incidents, often involving much greater stakes, led her to question: What does it mean to be a doctor if you can’t support your patients when they need you most?
This sentiment resonates deeply. Personally, I recall a time when our physicians were consistently available whenever we required assistance, from birth through later years, encompassing general surgical needs that excluded complex brain or heart surgeries. If they couldn’t attend personally, a nearby colleague would always step in. Back then, healthcare may not have been universal, but it was rare for anyone in need to go without care. As one internist friend succinctly noted, “We generally received our payments, but when we didn’t, it had a profound impact on our patients and their families.” We were delivering medical care as it was intended to be delivered.
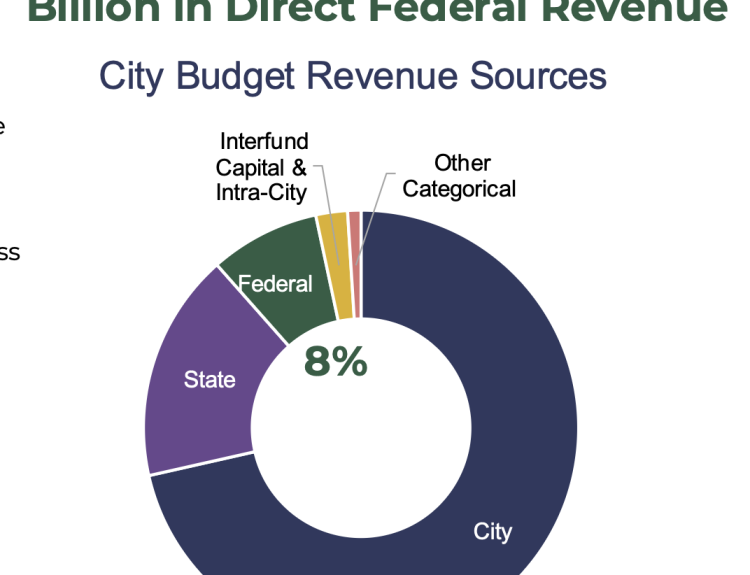
Looking forward, does primary care possess a viable future? It should, as its decline would reverberate through society, impacting those who rely on urgent care for medication refills and chronic illness management. This isn’t a sustainable trajectory, yet the decline seems unstoppable. What could possibly reverse this trend? An extensive investment in both time and resources could be part of the solution, considering that primary care currently garners less than 5% of U.S. healthcare expenditures, despite accounting for 35% of patient visits.
Nevertheless, there is a growing belief among the public—aside from those requiring a PCP—that primary care can be effectively delivered by advanced practice providers like nurse practitioners (NPs) and physician assistants (PAs). Some of my close friends were among the first PAs; their training was exceptional, and they provided quality care during their decades of practice under physician supervision. Likewise, the pioneering NPs delivered outstanding service. During my own cancer treatment, oncology NPs and nurses were crucial, working alongside a team of five oncologists and three radiation oncologists within a well-integrated practice. However, it’s unclear whether NPs and PAs in independent practices can adequately fill the gap left by the shortage of PCPs. Evidence suggests that the rigor of NP and PA training programs has diminished over the years.
More critically, the primary role of a PCP is to maintain a holistic understanding of patients through enduring and consistent contact, serving as the primary coordinator when multispecialty care is required. They act as captains guiding the care team. Without a cohesive leader, various specialists can function without connection, akin to a group of blind men each describing different parts of an elephant. While these specialists are vital to patient care—with my ENT, oncologists, and radiation specialists playing a crucial role in my recovery—it was my internist who first diagnosed my condition and set the treatment plan in motion. Despite the complexities introduced by contemporary hospital systems, my internist monitored my journey throughout, underscoring the collaborative effort that went into my care.
These dynamics invite reflection on what has been termed the “paradox of primary care”:
Even though individual patients receiving treatment from specialists achieve better disease-specific outcomes, population-level data imply that regions with a higher ratio of primary to specialty care demonstrate healthier populations, improved quality of services, greater equity, and lower costs… U.S. states with a higher concentration of generalists consistently spend less and provide more effective care than those with a heavier reliance on specialists. Others have noted that patients with multiple chronic conditions exhibit similar functional health statuses whether they are treated by generalists or specialists, yet generalists deploy fewer resources.
Of course, confounding factors may be at play that could influence these findings. Yet, a community that prioritizes investment in primary care is more likely to also support social services that enhance overall health:
Such limitations may become less significant than the prevalent belief that primary care’s actual worth can be adequately quantified at all. This misunderstanding is hastening its decline… Reinventing the system necessitates recognizing the inherent value of generalists—a recognition that is sorely lacking. Instead, primary care has been dissected into its revenue-generating components, leaving many PCPs unable to cultivate the enduring relationships essential for comprehensive care. The risk of extinction looms ominously. The ongoing relevance of primary care hinges on its ability to provide services that cannot be obtained from specialists, retail clinics, or virtual solutions. If its core relational aspect is lost, will the public seek alternative solutions for their health and well-being? In essence, will the intrinsic value of traditional primary care fade from our collective consciousness?
This is where the stark reality of neoliberal thought comes into play. [3] Neoliberalism has been characterized as the ideology where “the market dictates all values, including those that resist measurement.” In terms of health and well-being, this tenet is being increasingly challenged by proponents of holistic care.
This mindset… contributes to a widespread misunderstanding of primary care, which should serve the whole person from cradle to grave. This misunderstanding is leading to its demise. As Dr. Kurt Strange pointed out, “In striving to enhance parts of primary care, we’ve inadvertently jeopardized the entire system.”
Alongside this, the current influencer culture has rendered the concept of a long-term physician almost obsolete, as wearables claim to provide all necessary health data right on our smartphones. Just ask the Secretary of Health and Human Services.
However, an escape from the confines of commodified medicine may still be feasible. As Dr. Rosenbaum shares:
“Despite the widespread burnout among PCPs, one of the more unexpected insights from my reporting was the joy and fulfillment expressed by several rural PCPs I spoke with. Operating in resource-limited environments offers its challenges, but it also fosters creativity. For example, consider an uninsured patient grappling with severe heart failure, refusing hospitalization that might bankrupt him and jeopardize his farm. He devises a plan with his trusted doctor to come to the clinic daily for IV diuresis and regular weight and electrolyte evaluations. What about a woman with nephrotic syndrome unable to visit the nephrologist three hours away? Her physician communicates directly with the nephrologist and learns to manage her care himself. Is the satisfaction found by rural practitioners linked to their autonomy, the variety of cases they handle, and their pivotal role in their communities? Yes, likely all these elements. Above all, these providers “meet patients where they are,” regardless of circumstance. Sadly, most U.S. primary care practitioners, constrained by large healthcare organizations, have been denied this essential capability.
It’s no surprise: healthcare systems often profit off hospitalizations, specialty referrals, and extensive testing. As Larry Green, a family physician and esteemed professor at the University of Colorado, pointedly remarked, “Effective primary care is increasingly detrimental to business.”
I want to stress that the responsibility of rural primary care physicians is paramount; if they falter, their patients’ lives are at stake under the harsh realities of neoliberalism, which rigidly adheres to market principles—“If you’re unable to pay, go perish.” It’s uplifting to witness many of our graduates return home to fulfill this crucial role in their communities.
And indeed, by neoliberal standards, effective primary care may be detrimental to business interests. Yet, the pressing inquiry remains: “Whose business is at stake?” The interests of Big Medicine and Big Pharma are, undeniably. As climate change continues to alter conditions, it could be that a renewed focus on rural living and rural healthcare may provide a way forward.
And what has become of Dr. H, who started our narrative?
Dr. H and her colleagues addressed numerous emails to their practice leadership, outlining their frustrations over lack of staff support and inadequate communication, along with their feelings of letting their patients down. “I cannot, in good conscience and with regard to my oath as a physician, continue to practice in this manner,” Dr. H lamented. Unfortunately, her concerns seemed to be falling on deaf ears. One particularly disturbing message reflected her fears about the fundamental mindset guiding the future of primary care: “Perhaps this is what the administration desires,” Dr. H contemplated: “to replace those who know with those who do not understand, those [who] have been indoctrinated into a system that strips humanity from medical care.” Dr. H’s anguish epitomizes the modern paradox of primary care: if its survival hinges on the advocacy of both physicians and patients, then as authentic primary care becomes rarer, fewer will even recognize its absence.
Yet, some of us will remain aware of the void. While specialized care is indispensable, many of us are healthy today owing to its availability. However, primary care—defined as being of paramount importance and foundational to the practice of medicine—remains vital. Its absence would be felt across society.
One evening, as Dr. H was finalizing her notes, she had a troubling premonition about her health. “You often hear of doctors who genuinely care, those who pour their hearts into their work only to collapse from stress or heart attacks,” she shared. As she glanced at a flyer seeking physicians for a concierge practice, something clicked for her. “Perhaps this was a sign from the universe answering my prayers for a fulfilling career,” she said, and promptly picked up her phone to inquire further.
Interestingly, the family doctors of my youth—ranging from GPs to surgeons—practiced what today could be construed as “concierge medicine.” If you needed them, they were available. They also earned enough to occupy prominent positions within the local economy, comparable to a bank president or heirs to profitable local enterprises (at least until they mismanaged the businesses in subsequent generations). These physicians were integral community members, often seen as authorities while maintaining a deep connection with the people they served. One was even part of my father’s bowling league, and they sometimes fished together. Such relationships were commonplace, and many of those doctors experienced long and fulfilling careers from the 1950s through the 1990s.
In closing, Dr. Rosenbaum hints at her upcoming article: “Next time: Does concierge medicine spell a rebirth – or the death – of primary care.” I will be eagerly awaiting this discussion, as it promises to be intriguing.
Notes
[1] While my medical experiences are fortunate, they are not entirely unique. Up until I required a dermatologist and Mohs surgeon in my early 50s (largely due to our skincare choices decades prior), I had never seen a specialist. I frequently visited the Emergency Department, where one of my family doctors would come from their nearby home to tend to my needs.
[2] In light of the fact that many fellow Americans can only access care through emergency rooms — mandated by law to treat everyone — one could argue that Emergency Medicine fits the criteria of primary care as well. Often, these emergency rooms cater to “frequent flyers,” who are in dire need of ongoing primary care.
[3] The comprehensive neoliberalization of medical practice frequently escapes notice from many physicians I know. They readily acknowledge the challenges posed by large health systems that hinder their ability to provide patient care in accordance with the Hippocratic Oath.