Yves here. The findings from the well-structured, multi-country study discussed below present a surprising yet significant insight: individuals facing greater health challenges tend to show less support for enhanced healthcare provisions compared to those who are healthier. This raises questions: Does the reality of ill health lead to concerns that improved services will impose broader societal costs? Or does it reflect a general trend where communities that perceive themselves as having resources are more willing to invest in social safety nets?
The authors also emphasize a troubling trend emerging in the US: declining well-being is leading to reduced support for comprehensive medical programs, which in turn contributes to further deterioration in the overall health of the population.
By Marcello Antonini, Visiting Fellow, Health Policy Department, London School of Economics and Political Science; Research Fellow, Centre for Primary Care and Health Services Research, Department of Economics, University of Oxford; and Joan Costa-i-Font, Professor of Health Economics, London School of Economics and Political Science. Originally published at VoxEU
The quality of people’s lives is intricately linked to policy decisions surrounding healthcare access and funding, making it essential to understand how the public perceives fairness. This column explores how an individual’s health status, represented through exposure to the BCG vaccination, influences their views on equitable access to care and their willingness to pay higher taxes. Those in better health tend to be more supportive of fair healthcare financing and equal access to care, suggesting that enhancing the overall health of the population could strengthen public support for equitable health systems.
Fairness in healthcare extends beyond merely providing identical resources to all. In reality, people’s perceptions of ‘fair’ are influenced more by shared social norms and justice concepts rather than strict equality (Olsen 2011, Starmans et al. 2017). Generally, people accept certain inequalities when they believe the reasons for those disparities are valid but reject those that seem arbitrary or unfair. The healthcare sector vividly highlights these fairness concerns, as access and funding decisions directly impact quality of life and, in many cases, survival. As healthcare costs continue to rise, grasping public notions of fairness is increasingly crucial for policy formulation.
Healthy or Unhealthy Self-Interest?
A key unresolved question is how personal circumstances, particularly one’s health, shape attitudes toward equitable access to care and fair health financing. Evidence from the COVID-19 pandemic indicates that exposure to this crisis heightened aversion to inequality, especially among people not directly affected (Costa-Font et al. 2021), and encouraged vaccination, a pro-social behavior (Voth et al. 2021).
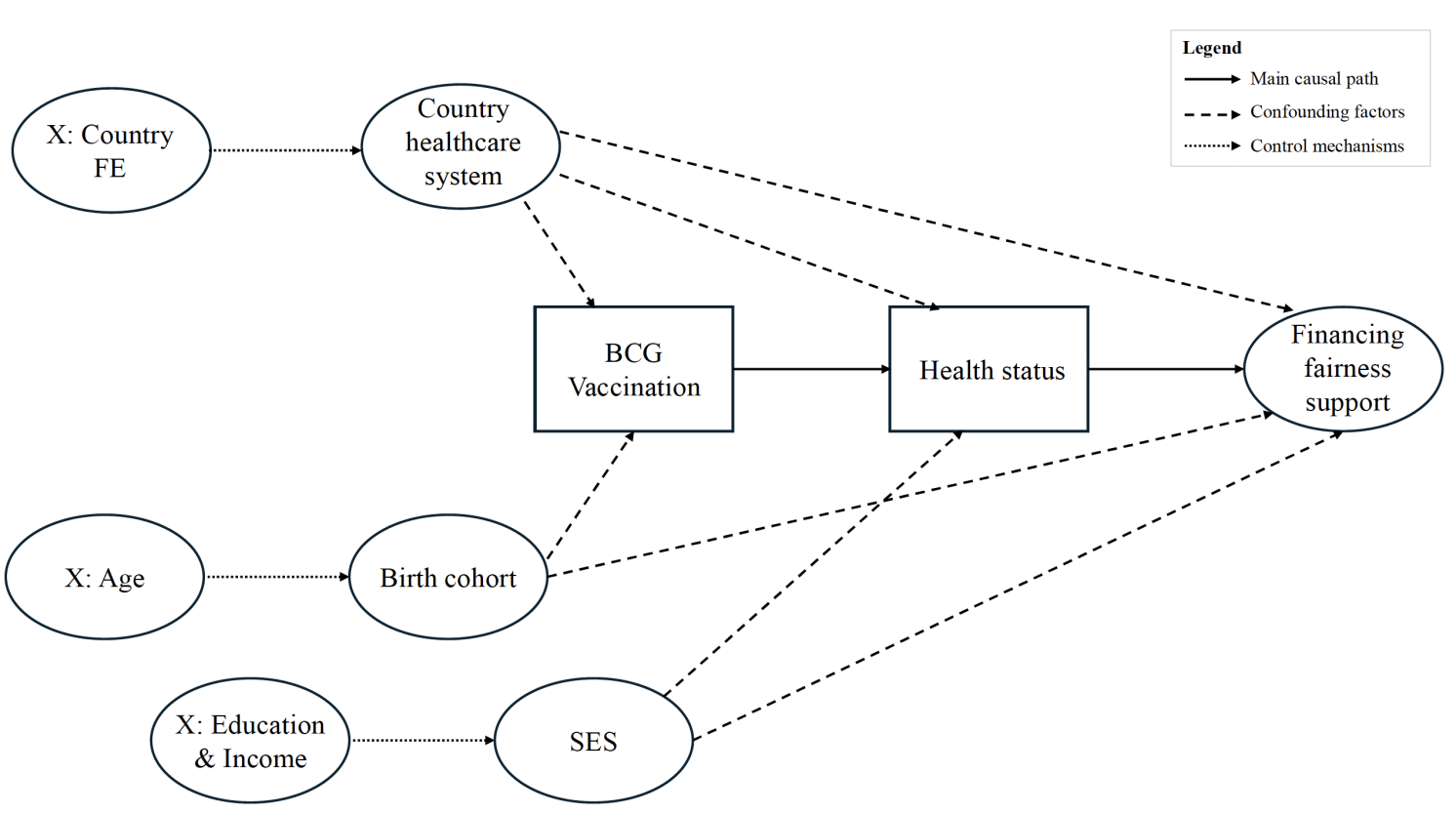
Figure 1 illustrates a directed acyclic graph that outlines our identification strategy, demonstrating the causal relationship from BCG vaccination to health status and preferences for financing fairness, while acknowledging possible confounding factors that our methodology addresses. We explore two competing hypotheses:
- The ‘healthy self-interest’ hypothesis posits that those in poor health are more inclined to support redistributive policies, as they stand to gain more from such measures, while healthier individuals may favor personal responsibility-based approaches.
- The ‘unhealthy self-interest’ hypothesis suggests the contrary: individuals in poor health may focus more on their immediate personal needs, hence displaying less concern for systemic fairness, whereas healthier individuals may possess a greater capacity to advocate for fairness norms.
Figure 1 Directed acyclic graph of the BCG vaccination instrumental-variable strategy
Health and Attitudes towards Health System Fairness
To explore the impact of health on perceptions of health system fairness, we conducted a study involving over 70,000 respondents from 22 countries. This analysis links self-reported health to attitudes towards equitable access and a willingness to finance enhanced public healthcare through higher taxes, as detailed in Antonini and Costa-Font (2025).
Figure 2 demonstrates a positive correlation between BCG vaccination exposure and preferences regarding financing fairness. Notably, the association is particularly strong for attitudes towards fair access, which yield higher average scores compared to willingness to support fair financing.
Figure 2 Association between BCG vaccination exposure and (1) attitudes toward fair access and (2) willingness to support fair financing, at the country level
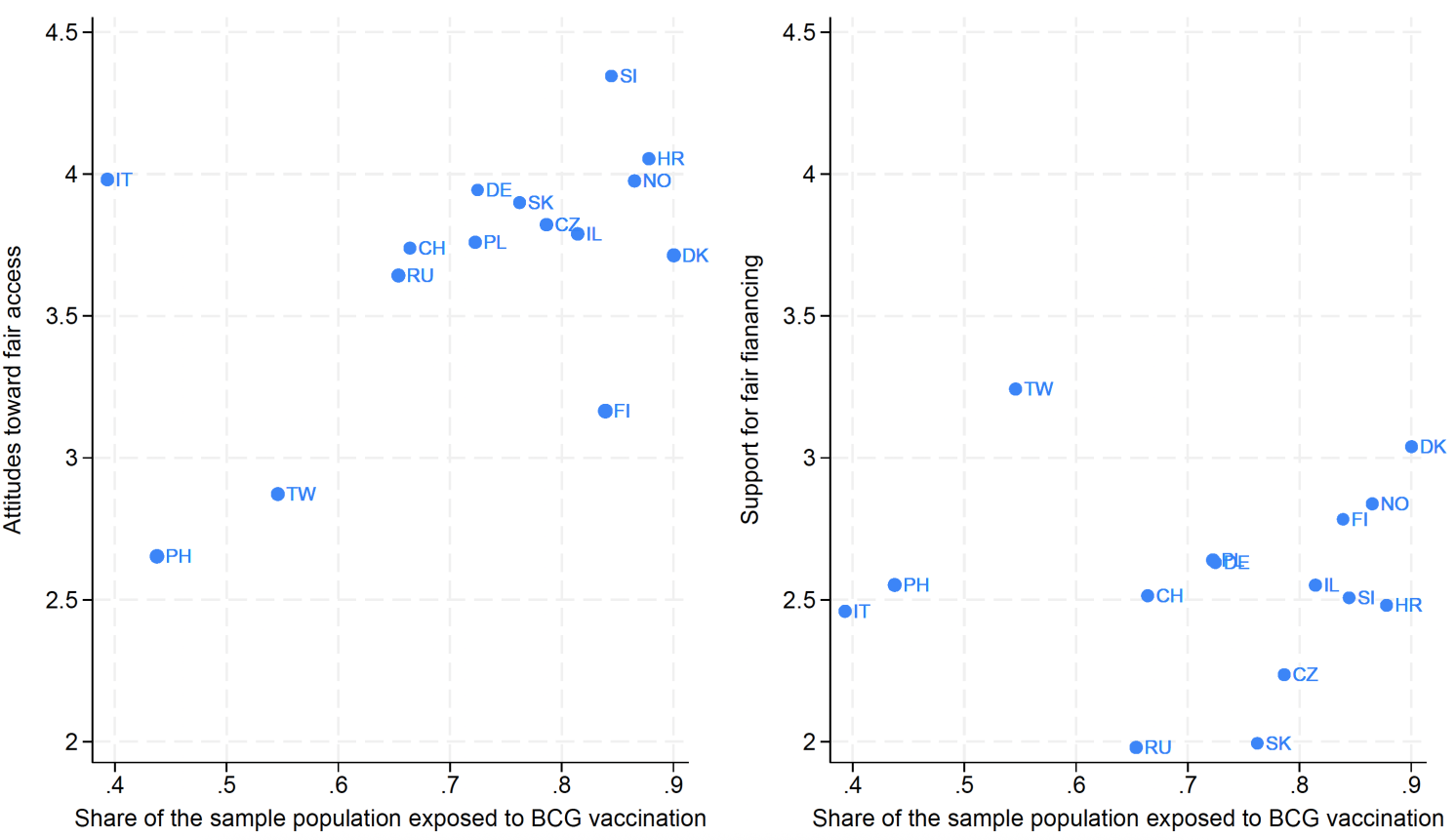
Notes: This figure displays a scatter plot correlating the instrument (exposure to the BCG vaccination) with the two outcomes: attitudes towards fair access (panel 1) and willingness to support fair financing (panel 2) at the national level. The size of the circles denotes the standard deviation for each outcome variable measured in each country. To create this scatter plot, we first computed the average levels of concern for both outcomes in every country and then plotted the mean values along the y-axis against the proportion of the population exposed to BCG vaccination along the x-axis.
Visual inspection of the graph suggests our instrument is a viable candidate for analysis. We derive causal estimates from an innovative instrumental-variable strategy based on variations in BCG vaccination exposure, enabling us to ascertain the causal impact of health status on fairness preferences. This methodology addresses the longstanding challenge of disentangling the influence of health from other social or economic factors.
The findings lend support to the ‘unhealthy self-interest’ hypothesis: individuals in poorer health exhibited lower support for fair health financing, while healthier individuals demonstrated stronger advocacy for both equal access and redistributive funding. An improvement of just one point in self-reported health corresponding to an 11% increase in support for fair access and an 8% increase in support for fair financing. This suggests that enhancing population health could not only improve well-being but also foster stronger public support for equitable health systems.
Our analysis indicates a more significant effect on normative judgments than on behavioral intentions that entail personal costs, pointing to a more pronounced influence of health status when financial sacrifice is not required. This pattern reveals that while healthier individuals show greater alignment with fairness principles, their support tends to wane when it necessitates actual financial contributions.
The mechanisms driving these effects primarily operate through economic channels (such as income and employment), with healthcare trust and political attitudes playing supplementary roles. This helps clarify why healthier individuals, who generally achieve better economic outcomes, exhibit stronger preferences for fairness in healthcare financing.
Moreover, these findings offer insight into why more unequal societies often face poorer health outcomes, including lower life expectancy, increased obesity rates, higher substance abuse, and worse mental health. Individuals suffering from ill-health tend to weaken their support for fairness in healthcare access and financing, making it less probable for policies aimed at enhancing equity to gain traction. Importantly, this trend appears across diverse healthcare systems, indicating a universal link between personal health and support for financing fairness, albeit with variations in strength by institutional context.
The causal relationship between better health and stronger support for fair healthcare financing hints at a potential virtuous cycle. As health systems effectively improve population health, public support for equitable policies may inherently grow. This dynamic may also shed light on why health inequalities occasionally resemble a Kuznets-type curve (Costa-Font et al. 2018). It further underscores the importance of investing in health improvements as a foundation for long-term equity. As health improves, systems may be better positioned to implement fairness-oriented allocation tools—like fairness weights—and prioritize historically marginalized groups whose needs become more apparent.
See original post for references

